
Tools and Shackles: Revisiting psychiatric medication…
Since I posted my piece on psychiatric drug promotion and the marketing of madness (the story of the Novartis DVD on Clozaril) I have had some really thought provoking and interesting, but also difficult, discussions with people who read and commented on my piece… Read more
‘A Journey into Light’? Psychiatric drug promotion and the marketing of madness
Last week, as part of carrying out research into women’s mental health at Manchester University, a colleague and I visited a Medium Secure Unit for women in the North West for a meeting to discuss some training for mental health nurses on the sexual and reproductive health of women accessing psychiatric care. Read more
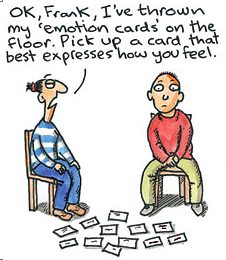
Humour…
Clare in the Community is a well known weekly cartoon by Harry Venning which appears every Wednesday in SocietyGuardian. The cartoon follows the trials and tribulations of Clare Barker, ‘a social worker with all the politically correct jargon but none of the practical solutions’, as described in the Guardian website. Read more
Reminders for 2013…
TO FELLOW SUFFERERS AND FELLOW TRAVELERS, JUST TO REMIND YOU…. Read more
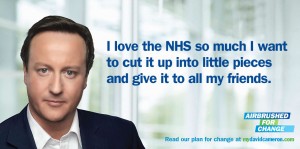
Timely political satire pointing to the imminent dismantling of the NHS…
In a speech back in May 2011, David Cameron apparently said: ‘It’s because I love the NHS so much that I want to change it. It needs to change to make it work better today and it needs to change to avoid a crisis tomorrow’ (London Evening Standard, 2011). MyDavidCameron website does political satire and published the poster below by Beau Bo D’Or: Read more
