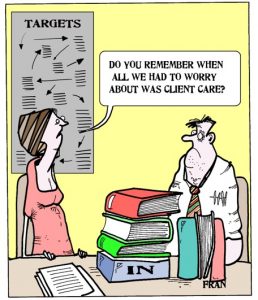
Where have ‘the good old days’ of mental health social work gone…when client care and support rather than an obsession with managerialist targets, outcomes and assessment against predetermined performance indicators and standards seemed to be the main concern and focus of mental health social work professionals?
Looking at the current socio-political and economic climate in the UK, the question as to where the ‘good old days’ of mental health social work have gone and the nostalgia surrounding it become increasingly poignant.
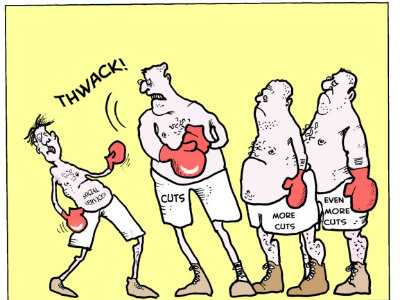
I am talking about the current climate of austerity cuts in both health/mental health services and the wider welfare state in the UK, where the operating conditions for mental health services are under immense pressure…
I am talking about mental health staff (including mental health social workers) working in disheartening and disempowering conditions characterised by job losses and staff shortages[1], excessive workloads, overcrowded wards[2]and drastic re-structuring of services that gives rise to increased uncertainty regarding the nature of mental health professionals’ roles…
I am talking about the acute sense of demoralisation, disempowerment and hopelessness in mental health professionals and service users alike that seems to be resulting from the disheartening and disempowering conditions within which mental health staff find themselves working…
I am talking about a time when we are witnessing a worrying rise in coercive practices in psychiatric services (Bentall, 2013) that seems to be reflected foremost in the rising tide of compulsory admissions to hospital and the growing use of Community Treatment Orders[3](Johnson, 2013). In way of illustration, compared with the previous year, 2012 saw a 5% increase in compulsory admissions to hospital, and a 10% increase in the use of Community Treatment Orders (Care Quality Commission, 2012).
In its recent report on the ‘Monitoring of the Mental Health Act in 2011/12’, the Care Quality Commission (2012) makes reference to the rise in coercive practices in psychiatric services by means of highlighting concerns that ‘cultures may persist [in inpatient wards] where control and containment are prioritised over the treatment and support of individuals’ (p.5).
Fran Cartoons
(www.communitycare.co.uk/blogs/mental-health/social-work-cartoon)
No wonder ‘the good old days’ of mental health social work are gone…when client care and support seemed to be the main concern and focus of mental health social work professionals…
_______________________________________________________________________________________
[1] Samuel, M. (2013) ‘Staff shortages mount among NHS mental health services’, 12 March. (www.communitycare.co.uk
[2] McNicoll, A. (2013) ‘Severe pressure’ on AMHPS amid job cuts, rising workload and bed shortages’, 30 January. (www.communitycare.co.uk)
[3] Community Treatment Orders (CTOs) – Certain patients subject to detention for treatment in hospital under the Mental Health Act 1983/2007 may be given a Community Treatment Order (CTO) upon discharge. CTOs contain conditions that patients have to comply with, including taking their medication, whilst living in the community. Failure to comply with these conditions entails that the patient could immediately be compulsorily readmitted to hospital (Lawton Smith, 2010).
Bentall, R. (2013) ‘Too much coercion in mental health services’, 1 February. (www.guardian.co.uk)
Care Quality Commission. (2012) Mental Health Act Annual Report 2011/12. http://www.cqc.org.uk/public/reports-surveys-and-reviews/reports/mental-health-act-annual-report-2011/12 [online resource] [accessed 090413].
Johnson, S. (2013) ‘Can we reverse the rising tide of compulsory admissions?’, The Lancet, Published online March 26, www.thelancet.com, http://dx.doi.org/10.1016/S0140-6736(13)60442-0
Lawton Smith, S. (2010) Supervised Community Treatment, Briefing Paper 2, London, Mental Health Alliance
