The Not Alone Collective are lived-experience activist artists and researchers based in Lanarkshire, Scotland.

They came together for the Scottish Mental Health Arts Festival 2023 after strongly identifying with its theme of ‘revolution’. They developed an innovative questionnaire about people’s adverse experiences with mental health practitioners based on a domestic violence checklist. This resulted in the creation of the Adverse Behaviours in Clinicians (ABC-11) as a much-needed tool in the prevention of harm towards those seeking healthcare.
Members of the Not Alone Collective originally met through mental health support groups and NHS services where we navigated our struggles with an unshakable sense of isolation. It took several years for us to realise the shared patterns of side effects, clinical negligence, and dearth of meaningful support we had all encountered. Discussions about harm inflicted by mental health staff and interventions were actively discouraged within both the NHS and third-sector services. The authoritarian narrative of mental health institutions placed the blame for poor treatment outcomes squarely on our shoulders, resulting in us internalising it as our fault. Scarcity of funding could explain some failings, but an otherwise unwavering reverence for the caring professions left service-users continually categorised as the ‘problem’ to be ‘fixed’.
Those engaging with support services were often left feeling alone, completely unaware that they were surrounded by true peers. Some individuals had been enduring the shame, confusion and pain caused by societal and systemic ‘othering’ for several years, for others it had been a lifetime. When the Mental Health Foundation announced the theme for their upcoming arts festival was ‘revolution’ one local community group gathered around a conference-style table and began finding strength through sharing stories and vulnerabilities. We came from a broad intersection of backgrounds, generations and lived-experiences. In being permitted to finally speak our truth, there were tears, despair, anger, dark humour and a palpable desire for change. Shame started to be replaced by hope.
However, just as solidarity was taking root, a facilitator became uncomfortable and reverted to enforcing the silencing required for toxic positivity to flourish. Their favouring of aesthetics over empowerment made it clear that any genuine revolution in the mental health sector would not come from within existing services. This realisation gave way to the Not Alone Collective.
Major news outlets are increasingly bringing to light instances of physical abuse suffered by inpatients and the tragic loss of lives while under the ‘care’ of mental health services. Public awareness of the potential harms of psychiatric medications is also on the rise. However, the power dynamic inherent in practitioner and service-user interactions, and the risks associated with talking therapies remain hidden. Non-pharmacological interventions are presumed safer, ‘gold standard’ and ‘evidence-based’, but often involve oversimplifying the causes of suffering and dogmatic approaches to recovery.
The quality of the therapeutic relationship has consistently been demonstrated as the most reliable determinant of positive outcomes within mental health care, regardless of discipline or therapy modality. Yet we discovered that between 33% and 65% of mental health professionals have been identified as ineffective or harmful in large-scale cross-disciplinary studies. In addition, up to 40% of individuals report finding no benefit from talk therapy and as many as 52.6% report negative outcomes, including side-effects and incidents of malpractice.
Well-being outcomes and access to effective support are also inconsistent across gender, race, disability and socio-economic class, with traditional approaches being found to perpetuate systems of oppression. With the current political climate inseparably influencing the sector, rhetoric and treatments that preserve the neoliberal status quo are favoured, regardless of their consequences on health. Systemic change will be slow to come and is already much too late for many. This leaves those relying on current services with no reassurances or guidance as to how to safely navigate towards appropriate care for their needs.
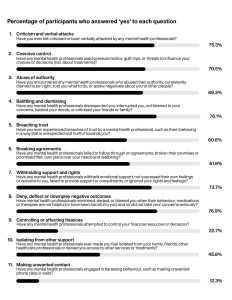
Therefore, we decided to embark on our own study, adopting a ‘back to basics’ approach that acknowledges power as the source of oppression and mistreatment. Drawing from our own experiences with mental health staff, we related to several items on a domestic violence resource which is used in the NHS to allow patients to identify harmful interpersonal behaviours in relationships. We realised it described how we had often been treated by practitioners and were curious to see if other people found it described their experiences too. Adapting the scenarios to apply to clinical mental health settings, we developed it into an eleven-item questionnaire that was sent out locally and online.
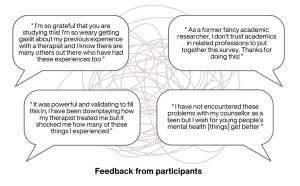
The response was overwhelming. 251 individuals participated in just three weeks. We received contributions from twenty-four countries, spanning experiences with nationalised, privatised, and charity-funded mental health services. While feedback from the broader community was validating, it also served as a painful reminder of the pervasiveness of epistemic injustice and harm.
The original domestic violence resource issued by the NHS advised that any of the behavioural scenarios they listed may indicate abuse in domestic relationships and a signal to reach out for help. It might be reasonable to assume that none of these would be found within a healthcare setting. Yet the table (at the end of this article) shows the percentage of participants who answered ‘yes’ to each question.
In total, 94% of respondents identified one or more of these in their interactions with mental health staff. On average, participants reported experiencing six out of eleven adversities, and this was consistent across locations (UK, USA, and EU) and service types. It is important to note that a questionnaire about adverse events will undoubtedly attract participation from individuals who have been negatively affected by these experiences. As such, the results do not claim that 94% of people have or will encounter these harmful behaviours when accessing mental health services.
We decided to formalise the questionnaire and call it the Adverse Behaviours in Clinicians (ABC-11) checklist, mirroring the style of clinical psychometric tests that are familiar to many. This user-led tool represents the first standardised method for identifying potentially harmful interpersonal actions within healthcare settings. Moreover, it is based on the same guidance that practitioners already expect service-users to apply to their domestic relationships.
The research aimed to validate the ABC-11 as a valuable resource, capable of assisting individuals to safely pursue meaningful support in an uncertain landscape where their rights and realities are regularly dismissed. That a prototype checklist now exists offers opportunities for its improvement in future studies, such as expanding the scenarios to include those involving overt/physical abuse, and fine-tuning the examples provided.
We believe that it could be helpful for academics and professionals to use it to help them identify and address harm and negligence in their research and practice. For example, they could apply the ABC-11 alongside collecting demographic information (gender, diagnosis, race, socio-economic status, disability), modality (CBT, psychodynamic, person-centred, somatic, pluralistic), and service/practitioner variables (residential, community, funding levels, training, workload).
While psychiatric and psychological treatments can help some individuals cope with distress, it is crucial to recognise that vulnerable people relying on mental health services are at significant risk of harm due to adverse practitioner behaviours. Our initial demonstration of the ABC-11 establishes a benchmark for care standards and serves as a vital means of validation, solidarity, and advocacy. We hope that it can empower service-users and their supporters to identify harmful situations that may lead to negative outcomes and improve access to safe, meaningful, rights-based mental health care. Finally, by speaking truth to power it dispels shame and ensures individuals know that they are not alone.
Instagram: @NotAloneCollective
Twitter: @Not_Alone_Co
The full report includes references to all the research mentioned in this article and a printable copy of the ABC-11 checklist.
Not Alone Collective (2024) Back to basics: Moderating iatrogenic harm by identifying and measuring mental health practitioner behaviours associated with interpersonal violence. Available HERE
This is a sample article from the Summer 2024 issue of Asylum [31:2]. To read more, Subscribe to Asylum Magazine

Leave a comment