
Madness, Violence and the Media by Hel Spandler
Back in 1993, the Zito Trust was formed by the wife of Jonathan Zito who was killed by Christopher Clunis in a London Underground station in 1992.

Back in 1993, the Zito Trust was formed by the wife of Jonathan Zito who was killed by Christopher Clunis in a London Underground station in 1992.

I have worked with several serious offenders during my career as a mental health nurse, some of whom had committed violent murders while experiencing extreme psychological disorder.

When I first saw the advert for the MSc in Mad Studies, I was feeling frustrated and stuck. After 20 years of watching peer support being increasingly co-opted by the mental health system, I desperately needed to reconnect with social movements and local activism. It was the first ever Master’s level Mad Studies course, which felt exciting to me. Read more
The Spring 2024 edition of Asylum magazine is out now.
Our front cover image – Liberation is not a seat at your table – is by Lea Cooper.
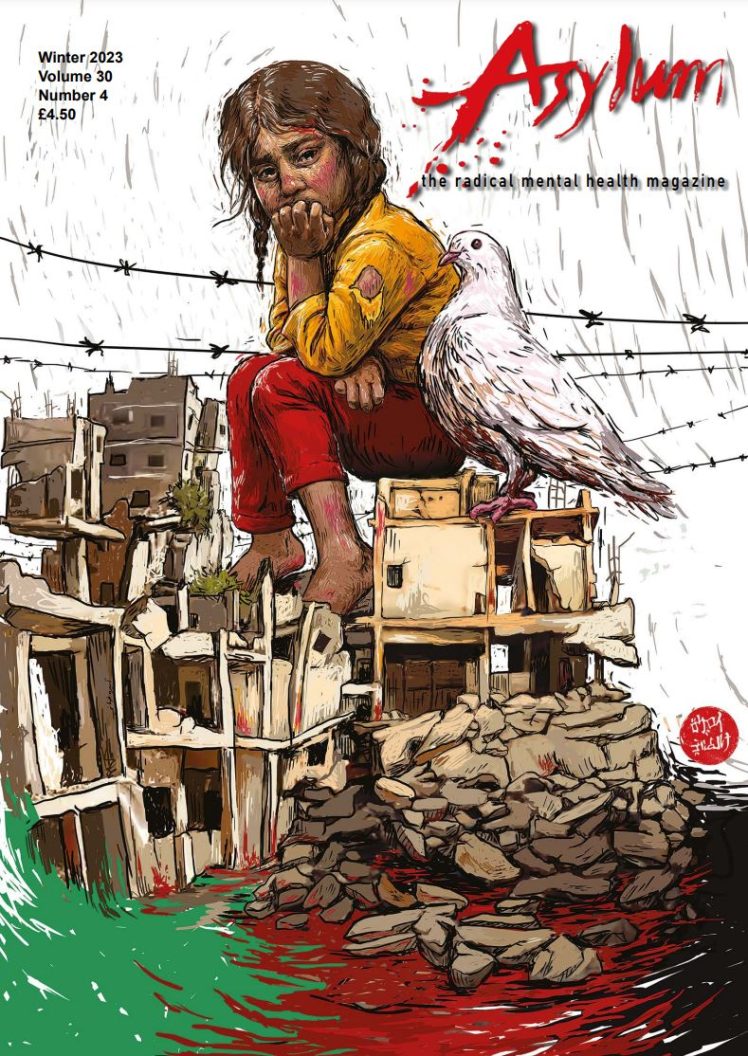
The Winter edition of Asylum magazine is out now. Our front cover image is ‘Childhood under Rubble’ by Amira Tanany.

We talk a lot about waste these days.